Why are people talking about ‘quadriceps-sparing’ (subvastus approach) or ‘muscle-sparing’ knee replacement and what is the difference between that and a ‘traditional’ parapatellar approach?
This is now my number one question in clinic so I figured I would answer it online to save you waiting until you can see me in person to ask it. From seeing many patients every day suffering with pain and poor mobility from knee arthritis, I can say confidently that the number one reason people avoid surgery is because they ‘know’ that knee replacements are very painful. They ‘know’ this because a friend/aunt/acquaintance/somebody on the internet had a knee replacement a number of years ago and it hurt.
But what if I told you that the recovery knee replacement doesn’t have to be as uncomfortable as it used to be? To be clear, knee replacement rehabilitation will still involve some discomfort, and the degree will vary from person to person in ways that are not always predictable. But it doesn’t have to be as bad as it once was- thanks to a combination of advances in muscle/tendon/ligament preservation, implants, anaesthetic techniques and postoperative pain minimisation with ice, elevation and less aggressive physiotherapy protocols.
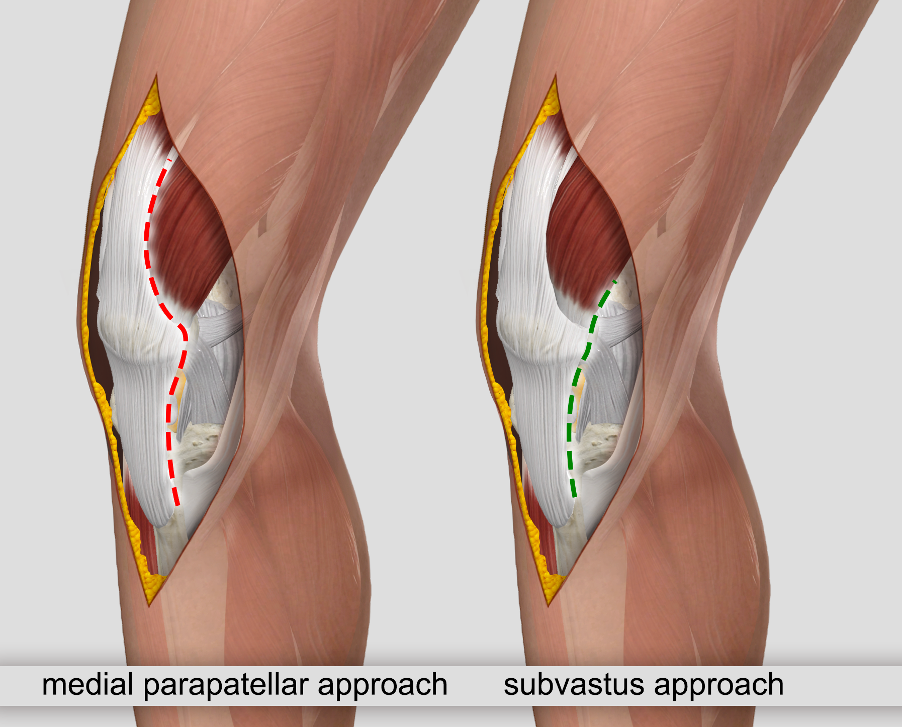
With the aim of reducing pain and speeding up recovery, some surgeons in the US and Europe and more recently some here in Australia have been performing knee replacements using a quadriceps-sparing technique. This technique avoids cutting any muscle/tendon and is called the ‘sub-vastus’ approach because it goes “sub” (underneath) the vastus medialis muscle, rather than cutting straight through the quadriceps tendon, which is how a traditional ‘medial parapatellar’ approach is executed as shown in the picture above.
Multiple research papers have shown that the subvastus approach offers less pain and faster recovery of range of motion (bending) in the first weeks after the procedure compared to a ‘traditional’ medial parapatellar approach (a meta-analysis of all these research papers was published in Journal of Arthroplasty 2023). Most of the benefit wears off by about 6 weeks postoperatively and the outcomes thereafter are largely the same regardless of approach. But it is those first couple of weeks after a knee replacement that are the worst part of the recovery for the patient so improving on that strikes me as a desirable aim.
Can all primary (first-time) knee replacements be done using this technique? Essentially yes. Some revision (re-do) knee replacements still have to be performed using a traditional parapatellar approach.
Unsurprisingly, there is a learning-curve associated with any transition to a new technique. The operations took me noticeably longer for the first 200 or so knee replacements I did with this new technique. Thankfully there were no notable complications for the patients, just longer operations and hence longer days for the surgeon and surgical team.
These are the two main reasons why not every surgeon adopts a quadriceps-sparing technique: each operation takes longer and it takes surgeons a while to get good at it. I’ve done over 500 knee replacements using this technique now so it now just feels as ‘normal’ as a major operation can really feel. And ultimately, however you get your knee replacement done, using a ‘quadriceps-sparing’ subvastus or ‘traditional’ medial parapatellar approach, you are getting the same implants and will end up with the same end outcome after a few months, it’s just a question of how you get there.